G2H2 Report on Financial Justice for Pandemic Prevention, Preparedness and Response (November 2022)
The G2H2 report: download PDF
Media release and resources: Media page
The report
A year ago, the second Special Session of the World Health Assembly (WHASS) unanimously agreed to start a diplomatic process for a new binding instrument aimed at ensuring the international community is better prepared for the next health emergencies. The establishment of an Intergovernmental Negotiating Body (INB) at the WHO paved the terrain for a proper negotiation, which has started to unfold. The INB will be releasing the “conceptual zero draft” of the treaty text in early December 2022.
Whatever the outcome of the process, one of the inescapable pillars of any new international agreement is addressing how to finance pandemic prevention, preparedness and response (PPR). This is the reason why the Geneva Global Health Hub (G2H2) decided to embark into the contentious relationship between the international financial architecture and current health financing models, towards highlighting the pitfalls the world must avoid to ensure a healthier post-COVID world.
There is no shortage of money in this world, but redirecting that money requires bold action. Most financial decisions rest with the G20 and fiscal policies with the OECD – entities with no jurisdiction that embody high-income countries’ interests. Therefore, we need delegates to get out of their silos and be prepared to confront the status quo, including actors and institutions that maintain the current system of global financial injustice. There are no easy solutions, but new ideas and initiatives at the UN are paving the way for addressing pathological relations of power at the root of health inequities.
The first section of the report scrutinizes the Pandemic Fund. Established at the initiative of the G20 in a rush to mobilize resources for PPR, its initial governance structure replicated the classical colonial paradigm. Low-income countries and civil society’s representation was allowed on its board only after strong and widespread criticism. With an outdated funding model dependent on colonial charity, the likely competition with other global health funds and very low expectations regarding its leverage on medical innovation, this cannot be the world’s solution to funding Pandemic PPR. Not even if its fundamental design flaws are repaired.
In its second section, the report demystifies two areas of financing solutions that have been implemented worldwide, pushed by the same neoliberal policy paradigm: fiscal consolidation and the commercialization of health services. Not only have the related policy measures failed to bring Health for All, in most cases they led to enhancing concentration of health and wealth in the hands of a few and a deterioration of health conditions for the vast majority of the population.
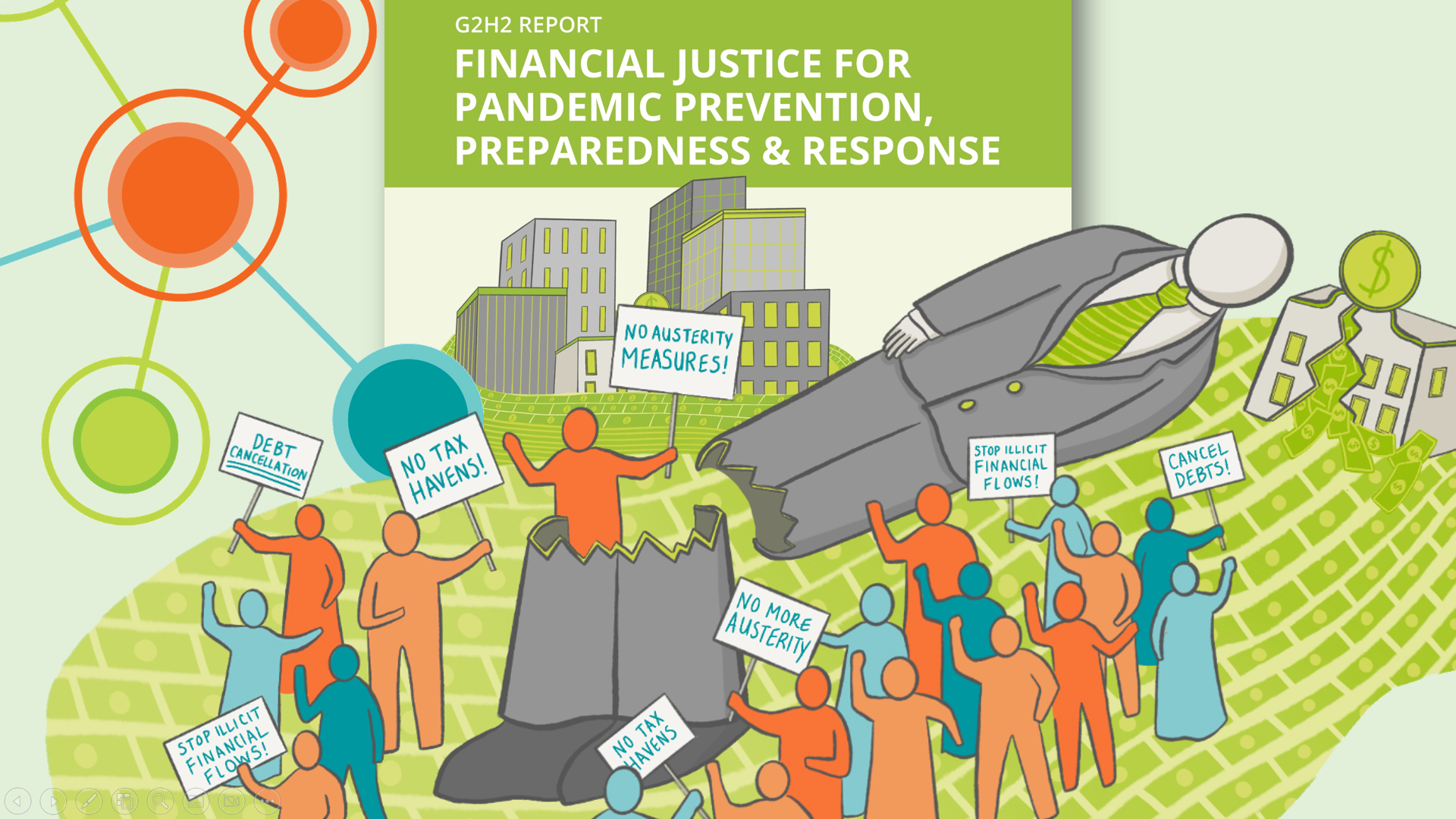
A historical analysis of the International Financial Institutions’ engagement shows how their push for economic reforms and austerity measures have led to reductions in health spending from the 1980s onwards. A sobering example is the IMF’s role in the Ebola outbreak rooted in the consequences of structural adjustment. To meet up with IMF conditionalities in the period leading to the 2014 Ebola emergency, Guinea, Liberia and Sierra Leone had been compelled to not only limit the number of health workers that they could hire, but also to cap health workers’ wages. After a brief spending boost during the Covid-19 pandemic, the IMF has now returned to pushing for ‘fiscal consolidation’ in country programs and loans. Despite its narrative of “abandoning austerity”, already in 2021, about 134 countries started cutting down on government spending and no less than 143 are projected to implement austerity measures by 2023.
Austerity goes hand in hand with commercialization and privatization of public services. Development actors’ promotion of privatization in low-income countries became stronger with the Washington Consensus in the 1990s and early 2000s. Yet, a solid body of evidence shows that public systems for healthcare delivery have overall been more efficient and effective, produce better healthcare outcomes, and perform better in terms of crisis prevention and preparedness. Astonishingly, since 2018 the World Bank Group is operationalizing its “private-first” approach through the so-called Maximizing Finance for Development strategy. Investments in health by the International Finance Corporation (IFC, the World Bank’s private sector arm) even ignore equitable access to services as a goal.
The third main part of this report leads the reader through the complex landscapes of debts and illicit financial flows. It is in these domains where a way out of the multiple crises must be sought. According to World Bank estimates, an additional 75-95 million people are being pushed into extreme poverty by the end of 2022, due to the unprecedented accumulation of financial pressures coming from the worsening debt crisis and the divergences in economic recovery plans from COVID-19. Research conducted on 41 countries shows that those with highest debt payments will spend an average 3% less on essential public services in 2023 than in 2019. The report demonstrates how the recipes offered by the G20, such as the Debt Service Suspension Initiative and the Common Framework, are not used and ultimately failing.
If the G20 and financial institutions had cancelled all external debts due in 2020 alone by the 76 lowest income countries, this would have liberated US$ 40 billion; US$ 300 billion if the cancellation had also included 2021. Arguments for a widespread debt write-off are clearly increasing, in the face of the global debt crisis. In fact, research shows how not only wealthy industrialized countries should pay the most to address climate change, but they should pay developing countries colossal reparations for the devastations provoked as historical emitters of greenhouses gases, causing US$ 6 trillion in global economic losses through warming from 1990 to 2014. Whose debt are we talking about, then?
Illicit Financial Flows (IFFs) are yet another drain on public resources that can only be tackled with radical action. According to UNCTAD, countries with high IFFs spend on average 25% less on health and around 50% less on education. Evidence suggests that the Eastern and Southern African region lost a staggering US$7.6 billion in tax revenue in 2017 alone, i.e. US$124.7 per capita, due to only two sources of IFFS (base erosion and profit shifting to tax havens). At the UN General Assembly in 2022, the Africa Group tabled a draft resolution calling for negotiations towards a UN convention on tax cooperation, building on the long-standing call by G77 & China to establish an intergovernmental process at the UN to address global tax abuse. This initiative should at least be receiving a strong indication of support in the context of the Intergovernmental Negotiating Body for the pandemic accord at the WHO.
These are the kind of unmentioned issues that need to be debated among WHO delegates when PPR financing makes its way on the agenda. In the emerging fragmented geopolitical landscape, WHO Member States – particularly from the global South – must find ways to converge on new essential instruments for financial justice. Such as stop paying for a debt, whose legitimacy must be questioned again, in view of global warming and climate change.
Civil society organizations, too, need to fully understand dynamics at play, and avoid being captured by this systemic injustice, as if it were a condition that cannot be repaired. The world needs a healthy financial system now. We encourage all the constituencies involved in the pandemic accord at the WHO, and those involved in other fora, to join the financial justice call that comes from the very UN system that the WHO belongs to.
(Executive Summary)
Launch of the report
G2H2 released its report “Financial Justice for Pandemic Prevention, Preparedness and Response” in a public event at the Geneva Press Club, on 15 November 2022. Ahead of the release of a zero draft of the WHO “pandemic treaty”, civil society experts and academics highlighted the urgent need to reshape and redirect financing towards prevention, preparedness and response to any future pandemics.
- Website of the launch event
Geneva, 15 November 2022
The G2H2 research and advocacy project that includes the publication of this report was sponsored by the Rosa-Luxemburg-Stiftung (RLS) with funds of the Federal Ministry for Economic Cooperation and Development of the Federal Republic of Germany. This report or parts of it can be used by others for free as long as they provide a proper reference to the original publication. The content of the publication is the sole responsibility of the Geneva Global Health Hub and does not necessarily reflect the position of RLS.
